
Wernig Laboratory
October 9, 2024: Welcome new postdoc Kirill to the lab!
Sep 17, 2024: Jinzhao's paper accepted in principle!
Jul 11, 2024: Gernot's paper published in Nature Communications!
March 21, 2024: Marius Mader's paper comes out in Nature Neuroscience!
Oct 10, 2023: Yongjin receives the Sammy Kuo Award from the Neuroscience Institute - CONGRATULATIONS!
Yongjin's paper on cell therapy in a mouse AD model is published in Cell Stem Cells
Our lab is generally interested in the molecular mechanisms that determine cell fates
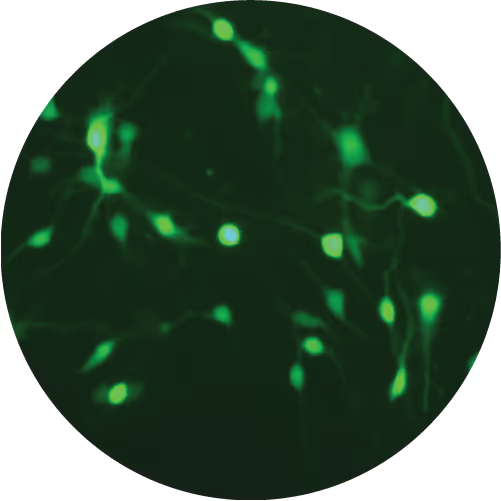
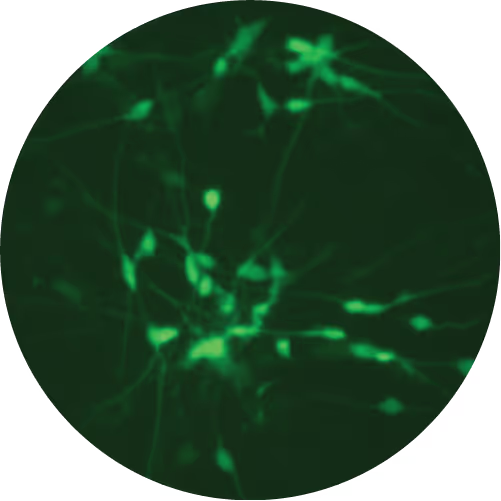
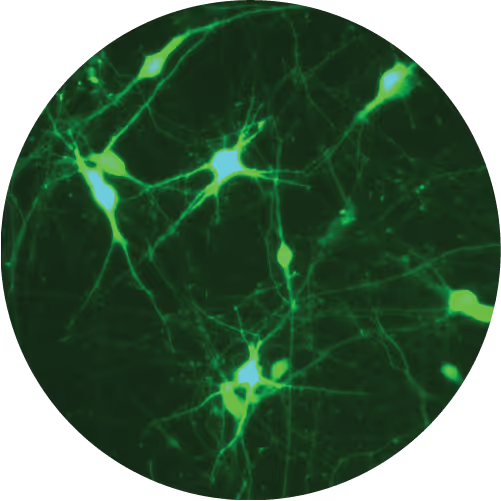
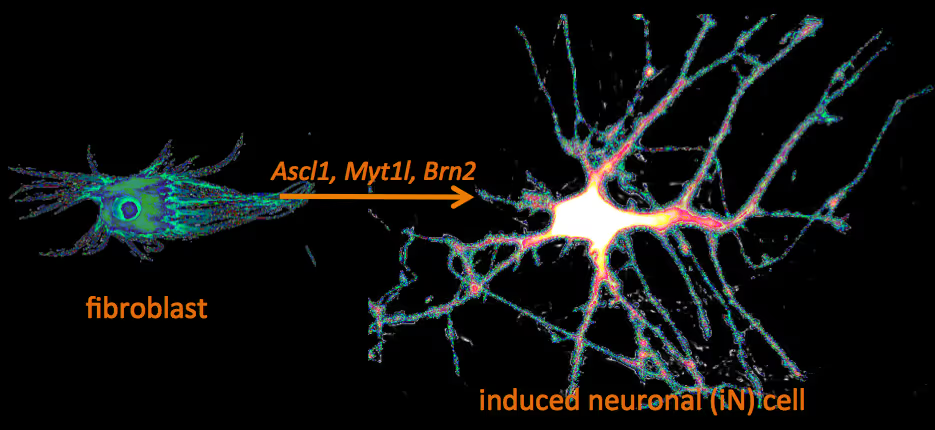
Recently, we have identified a pool of transcription factors that are sufficient to convert skin fibroblasts directly into functional neuronal cells that we termed induced neuronal (iN) cells. This was a surprising finding and indicated that direct lineage reprogramming may be applicable to many somatic cell types and many different directions. Indeed, following our work others have identified transcription factors that could induce cardiomyocytes, blood progenitors, and hepatocytes from fibroblasts.
We are now focussing on two major aspects of iN and iPS cell reprogramming:
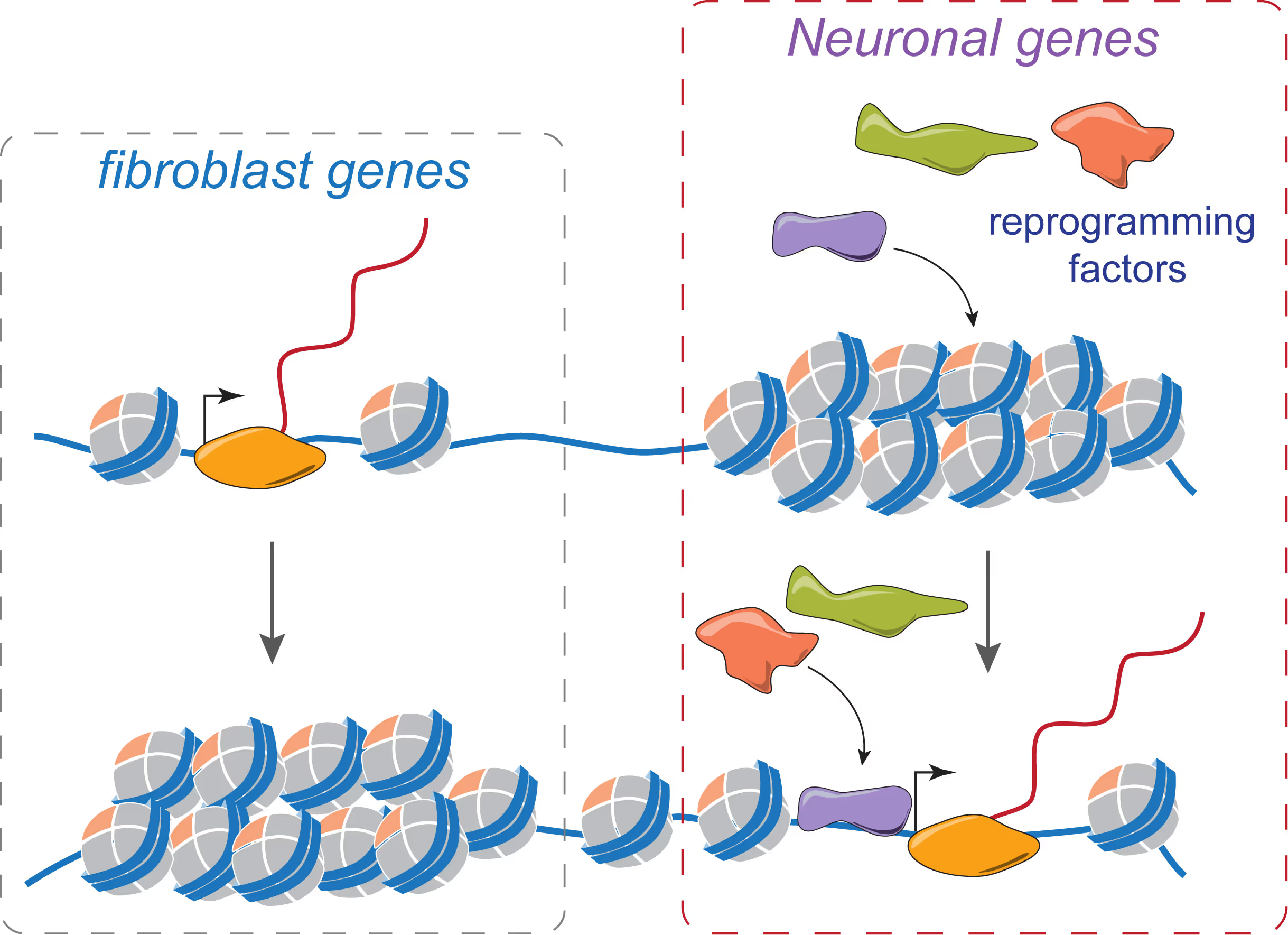
(i) we are fascinated by the puzzle how a hand full of transcription factors can so efficiently reprogram the entire epigenome of a cell so that it changes identity. To that end we are applying genome-wide expression analysis, chromatin immunoprecipitation, protein biochemistry, proteomics and functional screens.
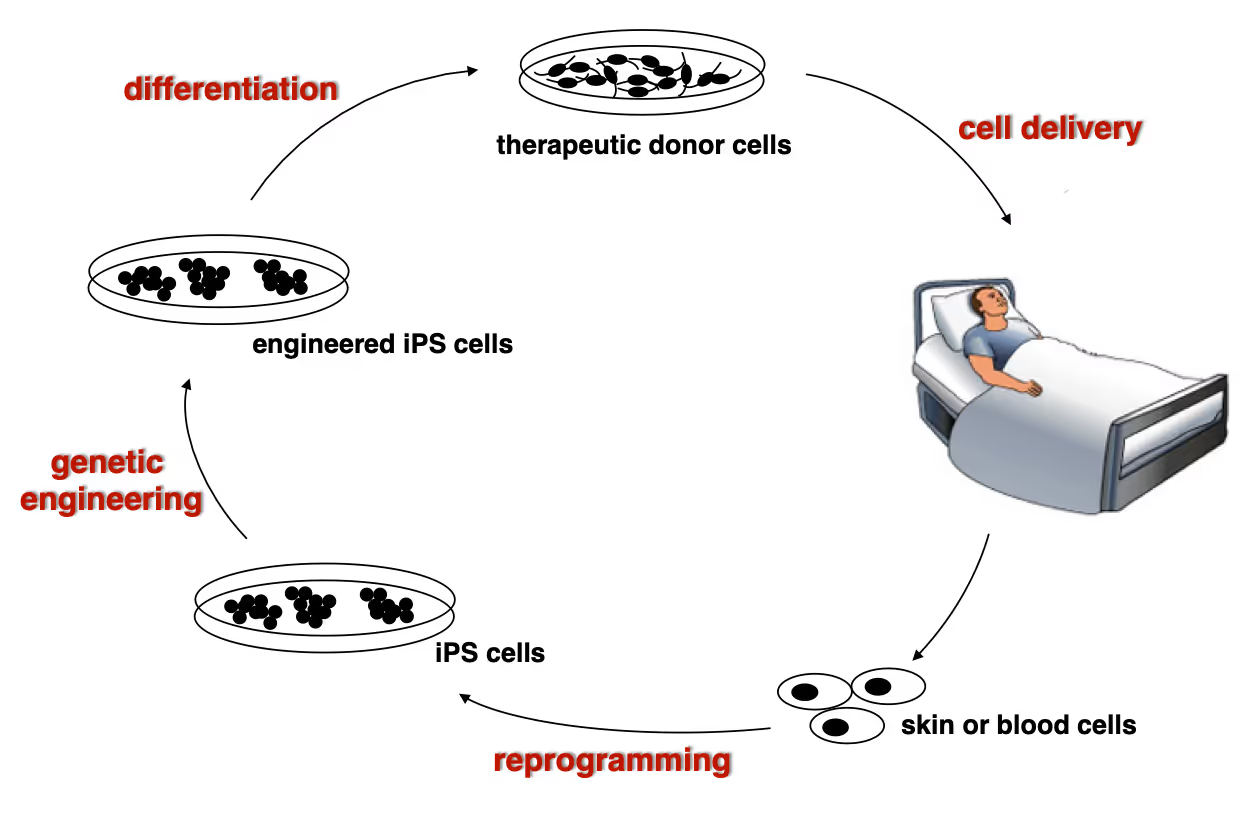
(ii) it is equally exciting to now use reprogramming methods as tools to study or treat certain diseases. iPS cells have the great advantage that they can easily be genetically manipulated rendering them ideal for treating monogenetic disorders when combined with cell transplantation-based therapies. In particular we are working on Dystrophic Epidermolysis Bullosa in collaboration with Stanford's Dermatology Department. An exciting application of iN cell technology will be to try modeling neurological diseases in vitro. We perform both mouse and human experiments hoping to identify quantifiable phenotypes correlated with genotype and in a second step evaluate whether this assay could be used to discover novel drugs improve the disease progression.
Wernig Lab Research
Overview
Our lab is interested in the molecular mechanisms that define neural lineage identity focusing on transcription factors and chromatin biology. We use cellular reprogramming to understand how neurons are induced, how they mature and maintain their identity. Reprogramming also allows us to generate a novel tool box to study human neuronal and glial cell biology which become powerful human disease models in combination with genetic engineering. We further seek to develop reprogramming & genetic engineering approaches towards stem cell-based therapies. Finally, we study microglia-neuron interactions with the ultimate goal to understand the brain's immune system in health and disease and to exploit microglia for therapeutic and regenerative purposes.
Human neuronal cell disease modeling
Neurosychiatric diseases like autism and schizophrenia are highly complex brain disorders difficult to model in mice in part due to complex genetic etiology and sometimes affecting human-specific genes. We develop novel human cell models to investigate disease-relevant cell biological phenomena.
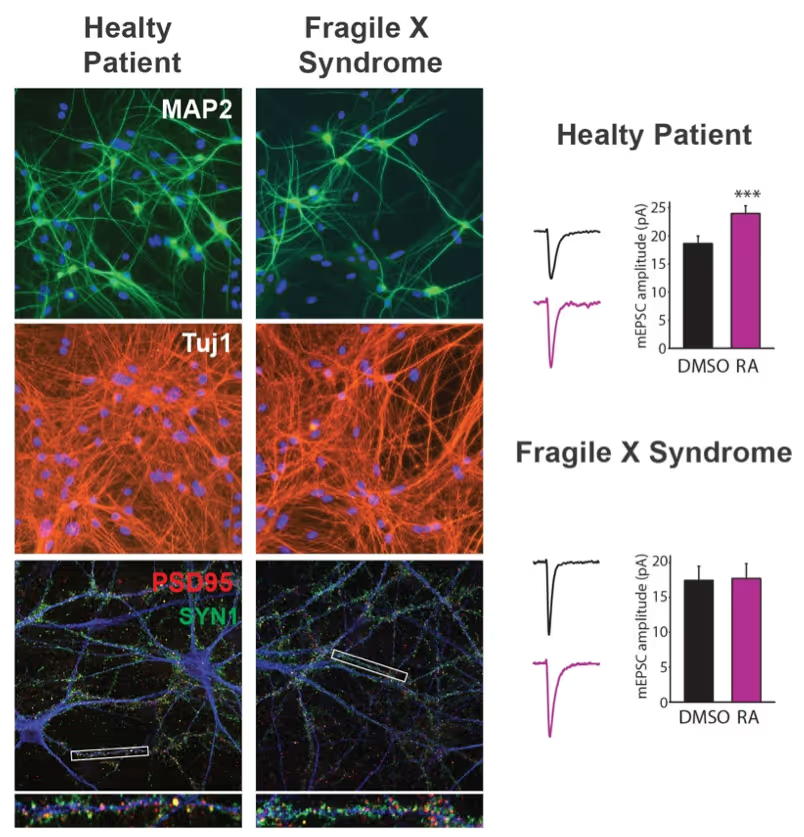
Generation of defined human neuronal cell types to study neuronal cell biology
We have and continue to develop protocols to generate specific types of neurons such as pure glutamatergic and pure GABAergic neurons from human pluripotent stem cells using transcription factors. In combination with genetic engineering or deriving iPS cells from patients, we then interrogate the cell biology of human neurons that carry disease-causing mutations. A particular focus is on synaptic function as shown in the figure on the right on Fragile X Syndrome neurons in collaboration with Lu Chen and Tom Südhof's laboratories.
Making neurons from blood
The ability to generate functional induced neuronal cells from distantly related somatic cell types is fascinating but also offers the opportunity to obtain neurons from a larger cohort of human subjects. In particular blood is readily available and we showed can be efficiently converted into functional neurons from young and aged donors.
Developing next generation cell therapies
The combination of reprogramming and gene editing is truly powerful as it provides exciting new possibilities to generate cells that can be transplanted and have disease modifying activity. We currently apply this approach to restore mono-genetic diseases, but our vision goes beyond simple regenerative medicine. We will be able to genetically engineer designer cells that functionally integrate into diseased tissue equipped with sensing and intelligent disease-response mechanisms.
Towards a Phase 1 clinical trial for the fatal skin disease Epidermolysis Bullosa
Dystrophic Epidermolysis Bullosa is a severe, blistering monogenetic skin disease caused by mutations in the gene coding for type VII collagen. We have developed a 1-step gene editing/iPS cell reprogramming method to rapidly generate patient iPS cells corrected for their disease-causing mutations in the Collagen7a1 gene. In collaboration with dermatologist Tony Oro we are developing a cell manufacturing process compatible with Good Manufacturing Procedures (GMP) to obtain FDA-approval for a first in man Phase I clinical trial with with a genetically engineered iPS cell product.
Exploiting glia cell transplantation to treat neurodegenerative disease
Both oligodendrocyte precursor cells as well as microglia can efficiently repopulate the brain. We are interested in exploiting the properties of these cells to develop novel cell therapies for the brain either to use the transplanted cells to restore function such as myelination, to alter the function of transplanted cells for therepeutic benefit, to use the cells as vehicles for therapeutic molecules, or ultimately to develop designer cells that are engineered with genetic synthetic biology circuits to sense and interfere with disease processes of the brain.
Mechanisms of neural cell lineage identity
We are interested in the molecular mechanisms that define neuronal and glial cell identity. We found sets of transcription factors that can convert fibroblasts or lymphocytes into neurons and oligodendrocytes. These factors are also operational during normal development and are largely responsible to induce terminal lineages from progenitor cells.
"On target" pioneer factors and chromatin remodeling during neuronal induction
We found that Ascl1, one of our reprogramming factors, has a unique ability to access its physiological targets even in fibroblasts where these sites are in a closed chromatin configuration. We are fascinated by this "on target" pioneering property and are investigating how Ascl1 can access its target sites in an unfavorable chromatin environment and how it then remodels the chromatin at these sites to activate the neuronal transcriptional program.
Maintenance of neuronal identity
Once neurons are made, there ought to be also mechanisms that maintain neuronal identity. We stumbled upon a novel repressive mechanism: The neuronal-specific transcription factor Myt1l continuosly represses many non-neuronal programs in neurons leaving the neuronal program open to activate by other factors and thereby ensuring stable neuronal gene expression. Myt1l was also recently found to be mutated in autism and schizophrenia.
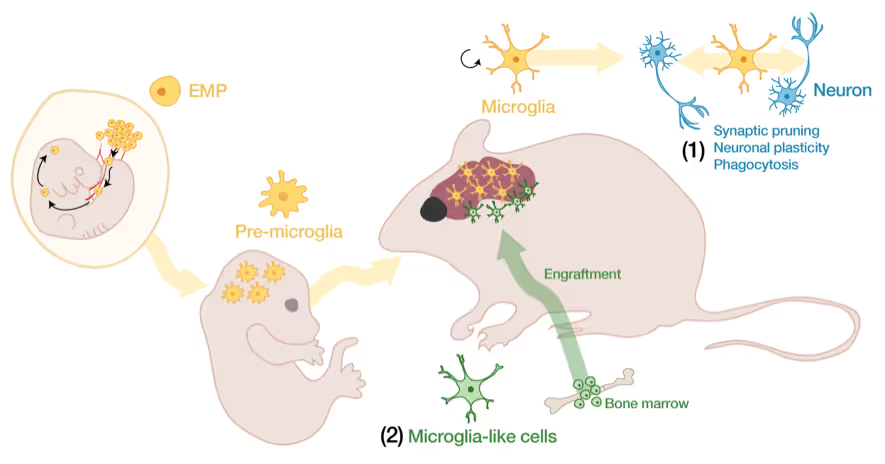
Microglia-neuron interactions in the healthy and diseased brain
Microglia, the brain's resident immune cells, are fascinating cells. They are derived from yolk sac progenitor cells early during development, are long-lived, and are not exchanged from bone marrow progenitor cells under physiological conditions. Microglia have been implicated in synaptic pruning, adult neurogenesis, and various brain diseases including Alzheimer's disease and Schizophrenia.
Developing an efficient microglia replacement system
We have developed a method to efficiently replace endogenous microglia from circulating cells without genetic manipulation. This does not happen physiologically but under certain conditions peripheral blood cells cross the blood-brain-barrier, migrate into the brain parenchyma and replace endogenous cells. We are investigating the cellular and molecular signals that enable circulating cells to invade the brain in order to further improve microglia replacement strategies.
The role of microglia in the normal and the diseased brain
Our ability to replace microglia provides us with a powerful tool to functionally perturb microglia function in normal and disease states. E.g. the microglial gene TREM2 is a strong Alzheimer's disease risk gene, but major questions about the neuro-immune interplay in the context of neurodegeneration and aging remain unsolved. Microglia replacement also provides an exciting prospect to develop novel cell therapies for a variety of brain diseases including enzyme deficiency syndromes, neurodegeneration, and brain tumors.
Lab Gene Expression Data
Publications
Mall M, Wernig M
Recent discoveries in the field of stem cell biology have enabled scientists to "reprogram" cells from one type to another. For example, it is now possible to place adult skin or blood cells in a dish and convert them into neurons, liver, or heart cells. It is also possible to literally "rejuvenate" adult cells by reprogramming them into embryonic-like stem cells, which in turn can be differentiated into every tissue and cell type of the human body. Our ability to reprogram cell types has four main implications for medicine: (1) scientists can now take skin or blood cells from patients and convert them to other cells to study disease processes. This disease modeling approach has the advantage over animal models because it is directly based on human patient cells. (2) Reprogramming could also be used as a "clinical trial in a dish" to evaluate the general efficacy and safety of newly developed drugs on human patient cells before they would be tested in animal models or people. (3) In addition, many drugs have deleterious side effects like heart arrhythmias in only a small and unpredictable subpopulation of patients. Reprogramming could facilitate precision medicine by testing the safety of already approved drugs first on reprogrammed patient cells in a personalized manner prior to administration. For example, drugs known to sometimes cause arrhythmias could be first tested on reprogrammed heart cells from individual patients. (4) Finally, reprogramming allows the generation of new tissues that could be grafted therapeutically to regenerate lost or damaged cells.
Recent discoveries in the field of stem cell biology have enabled scientists to "reprogram" cells from one type to another. For example, it is now possible to place adult skin or blood cells in a dish and convert them into neurons, liver, or heart cells. It is also possible to literally "rejuvenate" adult cells by reprogramming them into embryonic-like stem cells, which in turn can be differentiated into every tissue and cell type of the human body. Our ability to reprogram cell types has four main implications for medicine: (1) scientists can now take skin or blood cells from patients and convert them to other cells to study disease processes. This disease modeling approach has the advantage over animal models because it is directly based on human patient cells. (2) Reprogramming could also be used as a "clinical trial in a dish" to evaluate the general efficacy and safety of newly developed drugs on human patient cells before they would be tested in animal models or people. (3) In addition, many drugs have deleterious side effects like heart arrhythmias in only a small and unpredictable subpopulation of patients. Reprogramming could facilitate precision medicine by testing the safety of already approved drugs first on reprogrammed patient cells in a personalized manner prior to administration. For example, drugs known to sometimes cause arrhythmias could be first tested on reprogrammed heart cells from individual patients. (4) Finally, reprogramming allows the generation of new tissues that could be grafted therapeutically to regenerate lost or damaged cells.
Chuang W, Sharma A, Shukla P, Li G, Mall M, Rajarajan K, Abilez OJ, Hamaguchi R, Wu JC, Wernig M, Wu SM
Direct reprogramming of somatic cells has been demonstrated, however, it is unknown whether electrophysiologically-active somatic cells derived from separate germ layers can be interconverted. We demonstrate that partial direct reprogramming of mesoderm-derived cardiomyocytes into neurons is feasible, generating cells exhibiting structural and electrophysiological properties of both cardiomyocytes and neurons. Human and mouse pluripotent stem cell-derived CMs (PSC-CMs) were transduced with the neurogenic transcription factors Brn2, Ascl1, Myt1l and NeuroD. We found that CMs adopted neuronal morphologies as early as day 3 post-transduction while still retaining a CM gene expression profile. At week 1 post-transduction, we found that reprogrammed CMs expressed neuronal markers such as Tuj1, Map2, and NCAM. At week 3 post-transduction, mature neuronal markers such as vGlut and synapsin were observed. With single-cell qPCR, we temporally examined CM gene expression and observed increased expression of neuronal markers Dcx, Map2, and Tubb3. Patch-clamp analysis confirmed the neuron-like electrophysiological profile of reprogrammed CMs. This study demonstrates that PSC-CMs are amenable to partial neuronal conversion, yielding a population of cells exhibiting features of both neurons and CMs.
Direct reprogramming of somatic cells has been demonstrated, however, it is unknown whether electrophysiologically-active somatic cells derived from separate germ layers can be interconverted. We demonstrate that partial direct reprogramming of mesoderm-derived cardiomyocytes into neurons is feasible, generating cells exhibiting structural and electrophysiological properties of both cardiomyocytes and neurons. Human and mouse pluripotent stem cell-derived CMs (PSC-CMs) were transduced with the neurogenic transcription factors Brn2, Ascl1, Myt1l and NeuroD. We found that CMs adopted neuronal morphologies as early as day 3 post-transduction while still retaining a CM gene expression profile. At week 1 post-transduction, we found that reprogrammed CMs expressed neuronal markers such as Tuj1, Map2, and NCAM. At week 3 post-transduction, mature neuronal markers such as vGlut and synapsin were observed. With single-cell qPCR, we temporally examined CM gene expression and observed increased expression of neuronal markers Dcx, Map2, and Tubb3. Patch-clamp analysis confirmed the neuron-like electrophysiological profile of reprogrammed CMs. This study demonstrates that PSC-CMs are amenable to partial neuronal conversion, yielding a population of cells exhibiting features of both neurons and CMs.
Wapinski OL, Lee QY, Chen AC, Li R, Corces MR, Ang CE, Treutlein B, Xiang C, Baubet V, Suchy FP, Sankar V, Sim S, Quake SR, Dahmane N, Wernig M, Chang HY
How transcription factors (TFs) reprogram one cell lineage to another remains unclear. Here, we define chromatin accessibility changes induced by the proneural TF Ascl1 throughout conversion of fibroblasts into induced neuronal (iN) cells. Thousands of genomic loci are affected as early as 12 hr after Ascl1 induction. Surprisingly, over 80% of the accessibility changes occur between days 2 and 5 of the 3-week reprogramming process. This chromatin switch coincides with robust activation of endogenous neuronal TFs and nucleosome phasing of neuronal promoters and enhancers. Subsequent morphological and functional maturation of iN cells is accomplished with relatively little chromatin reconfiguration. By integrating chromatin accessibility and transcriptome changes, we built a network model of dynamic TF regulation during iN cell reprogramming and identified Zfp238, Sox8, and Dlx3 as key TFs downstream of Ascl1. These results reveal a singular, coordinated epigenomic switch during direct reprogramming, in contrast to stepwise cell fate transitions in development.
How transcription factors (TFs) reprogram one cell lineage to another remains unclear. Here, we define chromatin accessibility changes induced by the proneural TF Ascl1 throughout conversion of fibroblasts into induced neuronal (iN) cells. Thousands of genomic loci are affected as early as 12 hr after Ascl1 induction. Surprisingly, over 80% of the accessibility changes occur between days 2 and 5 of the 3-week reprogramming process. This chromatin switch coincides with robust activation of endogenous neuronal TFs and nucleosome phasing of neuronal promoters and enhancers. Subsequent morphological and functional maturation of iN cells is accomplished with relatively little chromatin reconfiguration. By integrating chromatin accessibility and transcriptome changes, we built a network model of dynamic TF regulation during iN cell reprogramming and identified Zfp238, Sox8, and Dlx3 as key TFs downstream of Ascl1. These results reveal a singular, coordinated epigenomic switch during direct reprogramming, in contrast to stepwise cell fate transitions in development.
Fantuzzo JA, De Filippis L, McGowan H, Yang N, Ng YH, Halikere A, Liu JJ, Hart RP, Wernig M, Zahn JD, Pang ZP
Neurocircuits in the human brain govern complex behavior and involve connections from many different neuronal subtypes from different brain regions. Recent advances in stem cell biology have enabled the derivation of patient-specific human neuronal cells of various subtypes for the study of neuronal function and disease pathology. Nevertheless, one persistent challenge using these human-derived neurons is the ability to reconstruct models of human brain circuitry. To overcome this obstacle, we have developed a compartmentalized microfluidic device, which allows for spatial separation of cell bodies of different human-derived neuronal subtypes (excitatory, inhibitory and dopaminergic) but is permissive to the spreading of projecting processes. Induced neurons (iNs) cultured in the device expressed pan-neuronal markers and subtype specific markers. Morphologically, we demonstrate defined synaptic contacts between selected neuronal subtypes by synapsin staining. Functionally, we show that excitatory neuronal stimulation evoked excitatory postsynaptic current responses in the neurons cultured in a separate chamber.
Neurocircuits in the human brain govern complex behavior and involve connections from many different neuronal subtypes from different brain regions. Recent advances in stem cell biology have enabled the derivation of patient-specific human neuronal cells of various subtypes for the study of neuronal function and disease pathology. Nevertheless, one persistent challenge using these human-derived neurons is the ability to reconstruct models of human brain circuitry. To overcome this obstacle, we have developed a compartmentalized microfluidic device, which allows for spatial separation of cell bodies of different human-derived neuronal subtypes (excitatory, inhibitory and dopaminergic) but is permissive to the spreading of projecting processes. Induced neurons (iNs) cultured in the device expressed pan-neuronal markers and subtype specific markers. Morphologically, we demonstrate defined synaptic contacts between selected neuronal subtypes by synapsin staining. Functionally, we show that excitatory neuronal stimulation evoked excitatory postsynaptic current responses in the neurons cultured in a separate chamber.
Mall M, Kareta MS, Chanda S, Ahlenius H, Perotti N, Zhou B, Grieder SD, Ge X, Drake S, Euong Ang C, Walker BM, Vierbuchen T, Fuentes DR, Brennecke P, Nitta KR, Jolma A, Steinmetz LM, Taipale J, Südhof TC, Wernig M
Normal differentiation and induced reprogramming require the activation of target cell programs and silencing of donor cell programs. In reprogramming, the same factors are often used to reprogram many different donor cell types. As most developmental repressors, such as RE1-silencing transcription factor (REST) and Groucho (also known as TLE), are considered lineage-specific repressors, it remains unclear how identical combinations of transcription factors can silence so many different donor programs. Distinct lineage repressors would have to be induced in different donor cell types. Here, by studying the reprogramming of mouse fibroblasts to neurons, we found that the pan neuron-specific transcription factor Myt1-like (Myt1l) exerts its pro-neuronal function by direct repression of many different somatic lineage programs except the neuronal program. The repressive function of Myt1l is mediated via recruitment of a complex containing Sin3b by binding to a previously uncharacterized N-terminal domain. In agreement with its repressive function, the genomic binding sites of Myt1l are similar in neurons and fibroblasts and are preferentially in an open chromatin configuration. The Notch signalling pathway is repressed by Myt1l through silencing of several members, including Hes1. Acute knockdown of Myt1l in the developing mouse brain mimicked a Notch gain-of-function phenotype, suggesting that Myt1l allows newborn neurons to escape Notch activation during normal development. Depletion of Myt1l in primary postmitotic neurons de-repressed non-neuronal programs and impaired neuronal gene expression and function, indicating that many somatic lineage programs are actively and persistently repressed by Myt1l to maintain neuronal identity. It is now tempting to speculate that similar 'many-but-one' lineage repressors exist for other cell fates; such repressors, in combination with lineage-specific activators, would be prime candidates for use in reprogramming additional cell types.
Normal differentiation and induced reprogramming require the activation of target cell programs and silencing of donor cell programs. In reprogramming, the same factors are often used to reprogram many different donor cell types. As most developmental repressors, such as RE1-silencing transcription factor (REST) and Groucho (also known as TLE), are considered lineage-specific repressors, it remains unclear how identical combinations of transcription factors can silence so many different donor programs. Distinct lineage repressors would have to be induced in different donor cell types. Here, by studying the reprogramming of mouse fibroblasts to neurons, we found that the pan neuron-specific transcription factor Myt1-like (Myt1l) exerts its pro-neuronal function by direct repression of many different somatic lineage programs except the neuronal program. The repressive function of Myt1l is mediated via recruitment of a complex containing Sin3b by binding to a previously uncharacterized N-terminal domain. In agreement with its repressive function, the genomic binding sites of Myt1l are similar in neurons and fibroblasts and are preferentially in an open chromatin configuration. The Notch signalling pathway is repressed by Myt1l through silencing of several members, including Hes1. Acute knockdown of Myt1l in the developing mouse brain mimicked a Notch gain-of-function phenotype, suggesting that Myt1l allows newborn neurons to escape Notch activation during normal development. Depletion of Myt1l in primary postmitotic neurons de-repressed non-neuronal programs and impaired neuronal gene expression and function, indicating that many somatic lineage programs are actively and persistently repressed by Myt1l to maintain neuronal identity. It is now tempting to speculate that similar 'many-but-one' lineage repressors exist for other cell fates; such repressors, in combination with lineage-specific activators, would be prime candidates for use in reprogramming additional cell types.
Chao MP, Gentles AJ, Chatterjee S, Lan F, Reinisch A, Corces MR, Xavy S, Shen J, Haag D, Chanda S, Sinha R, Morganti RM, Nishimura T, Ameen M, Wu H, Wernig M, Wu JC, Majeti R
Understanding the relative contributions of genetic and epigenetic abnormalities to acute myeloid leukemia (AML) should assist integrated design of targeted therapies. In this study, we generated induced pluripotent stem cells (iPSCs) from AML patient samples harboring MLL rearrangements and found that they retained leukemic mutations but reset leukemic DNA methylation/gene expression patterns. AML-iPSCs lacked leukemic potential, but when differentiated into hematopoietic cells, they reacquired the ability to give rise to leukemia in vivo and reestablished leukemic DNA methylation/gene expression patterns, including an aberrant MLL signature. Epigenetic reprogramming was therefore not sufficient to eliminate leukemic behavior. This approach also allowed us to study the properties of distinct AML subclones, including differential drug susceptibilities of KRAS mutant and wild-type cells, and predict relapse based on increased cytarabine resistance of a KRAS wild-type subclone. Overall, our findings illustrate the value of AML-iPSCs for investigating the mechanistic basis and clonal properties of human AML.
Understanding the relative contributions of genetic and epigenetic abnormalities to acute myeloid leukemia (AML) should assist integrated design of targeted therapies. In this study, we generated induced pluripotent stem cells (iPSCs) from AML patient samples harboring MLL rearrangements and found that they retained leukemic mutations but reset leukemic DNA methylation/gene expression patterns. AML-iPSCs lacked leukemic potential, but when differentiated into hematopoietic cells, they reacquired the ability to give rise to leukemia in vivo and reestablished leukemic DNA methylation/gene expression patterns, including an aberrant MLL signature. Epigenetic reprogramming was therefore not sufficient to eliminate leukemic behavior. This approach also allowed us to study the properties of distinct AML subclones, including differential drug susceptibilities of KRAS mutant and wild-type cells, and predict relapse based on increased cytarabine resistance of a KRAS wild-type subclone. Overall, our findings illustrate the value of AML-iPSCs for investigating the mechanistic basis and clonal properties of human AML.
Rivetti di Val Cervo P, Romanov RA, Spigolon G, Masini D, Martín-Montañez E, Toledo EM, La Manno G, Feyder M, Pifl C, Ng YH, Sánchez SP, Linnarsson S, Wernig M, Harkany T, Fisone G, Arenas E
Cell replacement therapies for neurodegenerative disease have focused on transplantation of the cell types affected by the pathological process. Here we describe an alternative strategy for Parkinson's disease in which dopamine neurons are generated by direct conversion of astrocytes. Using three transcription factors, NEUROD1, ASCL1 and LMX1A, and the microRNA miR218, collectively designated NeAL218, we reprogram human astrocytes in vitro, and mouse astrocytes in vivo, into induced dopamine neurons (iDANs). Reprogramming efficiency in vitro is improved by small molecules that promote chromatin remodeling and activate the TGFβ, Shh and Wnt signaling pathways. The reprogramming efficiency of human astrocytes reaches up to 16%, resulting in iDANs with appropriate midbrain markers and excitability. In a mouse model of Parkinson's disease, NeAL218 alone reprograms adult striatal astrocytes into iDANs that are excitable and correct some aspects of motor behavior in vivo, including gait impairments. With further optimization, this approach may enable clinical therapies for Parkinson's disease by delivery of genes rather than cells.
Cell replacement therapies for neurodegenerative disease have focused on transplantation of the cell types affected by the pathological process. Here we describe an alternative strategy for Parkinson's disease in which dopamine neurons are generated by direct conversion of astrocytes. Using three transcription factors, NEUROD1, ASCL1 and LMX1A, and the microRNA miR218, collectively designated NeAL218, we reprogram human astrocytes in vitro, and mouse astrocytes in vivo, into induced dopamine neurons (iDANs). Reprogramming efficiency in vitro is improved by small molecules that promote chromatin remodeling and activate the TGFβ, Shh and Wnt signaling pathways. The reprogramming efficiency of human astrocytes reaches up to 16%, resulting in iDANs with appropriate midbrain markers and excitability. In a mouse model of Parkinson's disease, NeAL218 alone reprograms adult striatal astrocytes into iDANs that are excitable and correct some aspects of motor behavior in vivo, including gait impairments. With further optimization, this approach may enable clinical therapies for Parkinson's disease by delivery of genes rather than cells.
Yang N, Chanda S, Marro S, Ng YH, Janas JA, Haag D, Ang CE, Tang Y, Flores Q, Mall M, Wapinski O, Li M, Ahlenius H, Rubenstein JL, Chang HY, Buylla AA, Südhof TC, Wernig M
Approaches to differentiating pluripotent stem cells (PSCs) into neurons currently face two major challenges-(i) generated cells are immature, with limited functional properties; and (ii) cultures exhibit heterogeneous neuronal subtypes and maturation stages. Using lineage-determining transcription factors, we previously developed a single-step method to generate glutamatergic neurons from human PSCs. Here, we show that transient expression of the transcription factors Ascl1 and Dlx2 (AD) induces the generation of exclusively GABAergic neurons from human PSCs with a high degree of synaptic maturation. These AD-induced neuronal (iN) cells represent largely nonoverlapping populations of GABAergic neurons that express various subtype-specific markers. We further used AD-iN cells to establish that human collybistin, the loss of gene function of which causes severe encephalopathy, is required for inhibitory synaptic function. The generation of defined populations of functionally mature human GABAergic neurons represents an important step toward enabling the study of diseases affecting inhibitory synaptic transmission.
Approaches to differentiating pluripotent stem cells (PSCs) into neurons currently face two major challenges-(i) generated cells are immature, with limited functional properties; and (ii) cultures exhibit heterogeneous neuronal subtypes and maturation stages. Using lineage-determining transcription factors, we previously developed a single-step method to generate glutamatergic neurons from human PSCs. Here, we show that transient expression of the transcription factors Ascl1 and Dlx2 (AD) induces the generation of exclusively GABAergic neurons from human PSCs with a high degree of synaptic maturation. These AD-induced neuronal (iN) cells represent largely nonoverlapping populations of GABAergic neurons that express various subtype-specific markers. We further used AD-iN cells to establish that human collybistin, the loss of gene function of which causes severe encephalopathy, is required for inhibitory synaptic function. The generation of defined populations of functionally mature human GABAergic neurons represents an important step toward enabling the study of diseases affecting inhibitory synaptic transmission.
Osorio MJ, Rowitch DH, Tesar P, Wernig M, Windrem MS, Goldman SA
Pelizaeus-Merzbacher disease (PMD) is an X-linked disorder caused by mutation in the proteolipid protein-1 (PLP1) gene, which encodes the proteolipid protein of myelinating oligodendroglia. PMD exhibits phenotypic variability that reflects its considerable genotypic heterogeneity, but all forms of the disease result in central hypomyelination, associated in most cases with early neurological dysfunction, progressive deterioration, and ultimately death. PMD may present as a connatal, classic and transitional forms, or as the less severe spastic paraplegia type 2 and PLP-null phenotypes. These disorders are most often associated with duplications of the PLP1 gene, but can also be caused by coding and noncoding point mutations as well as full or partial deletion of the gene. A number of genetically-distinct but phenotypically-similar disorders of hypomyelination exist which, like PMD, lack any effective therapy. Yet as relatively pure CNS hypomyelinating disorders, with limited involvement of the PNS and relatively little attendant neuronal pathology, PMD and similar hypomyelinating disorders are attractive therapeutic targets for neural stem cell and glial progenitor cell transplantation, efforts at which are now underway in a number of research centers. Stem Cells 2017;35:311-315.
Pelizaeus-Merzbacher disease (PMD) is an X-linked disorder caused by mutation in the proteolipid protein-1 (PLP1) gene, which encodes the proteolipid protein of myelinating oligodendroglia. PMD exhibits phenotypic variability that reflects its considerable genotypic heterogeneity, but all forms of the disease result in central hypomyelination, associated in most cases with early neurological dysfunction, progressive deterioration, and ultimately death. PMD may present as a connatal, classic and transitional forms, or as the less severe spastic paraplegia type 2 and PLP-null phenotypes. These disorders are most often associated with duplications of the PLP1 gene, but can also be caused by coding and noncoding point mutations as well as full or partial deletion of the gene. A number of genetically-distinct but phenotypically-similar disorders of hypomyelination exist which, like PMD, lack any effective therapy. Yet as relatively pure CNS hypomyelinating disorders, with limited involvement of the PNS and relatively little attendant neuronal pathology, PMD and similar hypomyelinating disorders are attractive therapeutic targets for neural stem cell and glial progenitor cell transplantation, efforts at which are now underway in a number of research centers. Stem Cells 2017;35:311-315.
Huang YA, Zhou B, Wernig M, Südhof TC
Human apolipoprotein E (ApoE) apolipoprotein is primarily expressed in three isoforms (ApoE2, ApoE3, and ApoE4) that differ only by two residues. ApoE4 constitutes the most important genetic risk factor for Alzheimer's disease (AD), ApoE3 is neutral, and ApoE2 is protective. How ApoE isoforms influence AD pathogenesis, however, remains unclear. Using ES-cell-derived human neurons, we show that ApoE secreted by glia stimulates neuronal Aβ production with an ApoE4 > ApoE3 > ApoE2 potency rank order. We demonstrate that ApoE binding to ApoE receptors activates dual leucine-zipper kinase (DLK), a MAP-kinase kinase kinase that then activates MKK7 and ERK1/2 MAP kinases. Activated ERK1/2 induces cFos phosphorylation, stimulating the transcription factor AP-1, which in turn enhances transcription of amyloid-β precursor protein (APP) and thereby increases amyloid-β levels. This molecular mechanism also regulates APP transcription in mice in vivo. Our data describe a novel signal transduction pathway in neurons whereby ApoE activates a non-canonical MAP kinase cascade that enhances APP transcription and amyloid-β synthesis.
Human apolipoprotein E (ApoE) apolipoprotein is primarily expressed in three isoforms (ApoE2, ApoE3, and ApoE4) that differ only by two residues. ApoE4 constitutes the most important genetic risk factor for Alzheimer's disease (AD), ApoE3 is neutral, and ApoE2 is protective. How ApoE isoforms influence AD pathogenesis, however, remains unclear. Using ES-cell-derived human neurons, we show that ApoE secreted by glia stimulates neuronal Aβ production with an ApoE4 > ApoE3 > ApoE2 potency rank order. We demonstrate that ApoE binding to ApoE receptors activates dual leucine-zipper kinase (DLK), a MAP-kinase kinase kinase that then activates MKK7 and ERK1/2 MAP kinases. Activated ERK1/2 induces cFos phosphorylation, stimulating the transcription factor AP-1, which in turn enhances transcription of amyloid-β precursor protein (APP) and thereby increases amyloid-β levels. This molecular mechanism also regulates APP transcription in mice in vivo. Our data describe a novel signal transduction pathway in neurons whereby ApoE activates a non-canonical MAP kinase cascade that enhances APP transcription and amyloid-β synthesis.
Chanda S, Aoto J, Lee SJ, Wernig M, Südhof TC
Neuroligins are postsynaptic cell-adhesion molecules that bind to presynaptic neurexins. Although the general synaptic role of neuroligins is undisputed, their specific functions at a synapse remain unclear, even controversial. Moreover, many neuroligin gene mutations were associated with autism, but the pathophysiological relevance of these mutations is often unknown, and their mechanisms of action uninvestigated. Here, we examine the synaptic effects of an autism-associated neuroligin-4 substitution (called R704C), which mutates a cytoplasmic arginine residue that is conserved in all neuroligins. We show that the R704C mutation, when introduced into neuroligin-3, enhances the interaction between neuroligin-3 and AMPA receptors, increases AMPA-receptor internalization and decreases postsynaptic AMPA-receptor levels. When introduced into neuroligin-4, conversely, the R704C mutation unexpectedly elevated AMPA-receptor-mediated synaptic responses. These results suggest a general functional link between neuroligins and AMPA receptors, indicate that both neuroligin-3 and -4 act at excitatory synapses but perform surprisingly distinct functions, and demonstrate that the R704C mutation significantly impairs the normal function of neuroligin-4, thereby validating its pathogenicity.
Neuroligins are postsynaptic cell-adhesion molecules that bind to presynaptic neurexins. Although the general synaptic role of neuroligins is undisputed, their specific functions at a synapse remain unclear, even controversial. Moreover, many neuroligin gene mutations were associated with autism, but the pathophysiological relevance of these mutations is often unknown, and their mechanisms of action uninvestigated. Here, we examine the synaptic effects of an autism-associated neuroligin-4 substitution (called R704C), which mutates a cytoplasmic arginine residue that is conserved in all neuroligins. We show that the R704C mutation, when introduced into neuroligin-3, enhances the interaction between neuroligin-3 and AMPA receptors, increases AMPA-receptor internalization and decreases postsynaptic AMPA-receptor levels. When introduced into neuroligin-4, conversely, the R704C mutation unexpectedly elevated AMPA-receptor-mediated synaptic responses. These results suggest a general functional link between neuroligins and AMPA receptors, indicate that both neuroligin-3 and -4 act at excitatory synapses but perform surprisingly distinct functions, and demonstrate that the R704C mutation significantly impairs the normal function of neuroligin-4, thereby validating its pathogenicity.
Carlson AL, Bennett NK, Francis NL, Halikere A, Clarke S, Moore JC, Hart RP, Paradiso K, Wernig M, Kohn J, Pang ZP, Moghe PV
Cell replacement therapy with human pluripotent stem cell-derived neurons has the potential to ameliorate neurodegenerative dysfunction and central nervous system injuries, but reprogrammed neurons are dissociated and spatially disorganized during transplantation, rendering poor cell survival, functionality and engraftment in vivo. Here, we present the design of three-dimensional (3D) microtopographic scaffolds, using tunable electrospun microfibrous polymeric substrates that promote in situ stem cell neuronal reprogramming, neural network establishment and support neuronal engraftment into the brain. Scaffold-supported, reprogrammed neuronal networks were successfully grafted into organotypic hippocampal brain slices, showing an ∼ 3.5-fold improvement in neurite outgrowth and increased action potential firing relative to injected isolated cells. Transplantation of scaffold-supported neuronal networks into mouse brain striatum improved survival ∼ 38-fold at the injection site relative to injected isolated cells, and allowed delivery of multiple neuronal subtypes. Thus, 3D microscale biomaterials represent a promising platform for the transplantation of therapeutic human neurons with broad neuro-regenerative relevance.
Cell replacement therapy with human pluripotent stem cell-derived neurons has the potential to ameliorate neurodegenerative dysfunction and central nervous system injuries, but reprogrammed neurons are dissociated and spatially disorganized during transplantation, rendering poor cell survival, functionality and engraftment in vivo. Here, we present the design of three-dimensional (3D) microtopographic scaffolds, using tunable electrospun microfibrous polymeric substrates that promote in situ stem cell neuronal reprogramming, neural network establishment and support neuronal engraftment into the brain. Scaffold-supported, reprogrammed neuronal networks were successfully grafted into organotypic hippocampal brain slices, showing an ∼ 3.5-fold improvement in neurite outgrowth and increased action potential firing relative to injected isolated cells. Transplantation of scaffold-supported neuronal networks into mouse brain striatum improved survival ∼ 38-fold at the injection site relative to injected isolated cells, and allowed delivery of multiple neuronal subtypes. Thus, 3D microscale biomaterials represent a promising platform for the transplantation of therapeutic human neurons with broad neuro-regenerative relevance.
Ahlenius H, Chanda S, Webb AE, Yousif I, Karmazin J, Prusiner SB, Brunet A, Südhof TC, Wernig M
We and others have shown that embryonic and neonatal fibroblasts can be directly converted into induced neuronal (iN) cells with mature functional properties. Reprogramming of fibroblasts from adult and aged mice, however, has not yet been explored in detail. The ability to generate fully functional iN cells from aged organisms will be particularly important for in vitro modeling of diseases of old age. Here, we demonstrate production of functional iN cells from fibroblasts that were derived from mice close to the end of their lifespan. iN cells from aged mice had apparently normal active and passive neuronal membrane properties and formed abundant synaptic connections. The reprogramming efficiency gradually decreased with fibroblasts derived from embryonic and neonatal mice, but remained similar for fibroblasts from postnatal mice of all ages. Strikingly, overexpression of a transcription factor, forkhead box O3 (FoxO3), which is implicated in aging, blocked iN cell conversion of embryonic fibroblasts, whereas knockout or knockdown of FoxO3 increased the reprogramming efficiency of adult-derived but not of embryonic fibroblasts and also enhanced functional maturation of resulting iN cells. Hence, FoxO3 has a central role in the neuronal reprogramming susceptibility of cells, and the importance of FoxO3 appears to change during development.
We and others have shown that embryonic and neonatal fibroblasts can be directly converted into induced neuronal (iN) cells with mature functional properties. Reprogramming of fibroblasts from adult and aged mice, however, has not yet been explored in detail. The ability to generate fully functional iN cells from aged organisms will be particularly important for in vitro modeling of diseases of old age. Here, we demonstrate production of functional iN cells from fibroblasts that were derived from mice close to the end of their lifespan. iN cells from aged mice had apparently normal active and passive neuronal membrane properties and formed abundant synaptic connections. The reprogramming efficiency gradually decreased with fibroblasts derived from embryonic and neonatal mice, but remained similar for fibroblasts from postnatal mice of all ages. Strikingly, overexpression of a transcription factor, forkhead box O3 (FoxO3), which is implicated in aging, blocked iN cell conversion of embryonic fibroblasts, whereas knockout or knockdown of FoxO3 increased the reprogramming efficiency of adult-derived but not of embryonic fibroblasts and also enhanced functional maturation of resulting iN cells. Hence, FoxO3 has a central role in the neuronal reprogramming susceptibility of cells, and the importance of FoxO3 appears to change during development.
Treutlein B, Lee QY, Camp JG, Mall M, Koh W, Shariati SA, Sim S, Neff NF, Skotheim JM, Wernig M, Quake SR
Direct lineage reprogramming represents a remarkable conversion of cellular and transcriptome states. However, the intermediate stages through which individual cells progress during reprogramming are largely undefined. Here we use single-cell RNA sequencing at multiple time points to dissect direct reprogramming from mouse embryonic fibroblasts to induced neuronal cells. By deconstructing heterogeneity at each time point and ordering cells by transcriptome similarity, we find that the molecular reprogramming path is remarkably continuous. Overexpression of the proneural pioneer factor Ascl1 results in a well-defined initialization, causing cells to exit the cell cycle and re-focus gene expression through distinct neural transcription factors. The initial transcriptional response is relatively homogeneous among fibroblasts, suggesting that the early steps are not limiting for productive reprogramming. Instead, the later emergence of a competing myogenic program and variable transgene dynamics over time appear to be the major efficiency limits of direct reprogramming. Moreover, a transcriptional state, distinct from donor and target cell programs, is transiently induced in cells undergoing productive reprogramming. Our data provide a high-resolution approach for understanding transcriptome states during lineage differentiation.
Direct lineage reprogramming represents a remarkable conversion of cellular and transcriptome states. However, the intermediate stages through which individual cells progress during reprogramming are largely undefined. Here we use single-cell RNA sequencing at multiple time points to dissect direct reprogramming from mouse embryonic fibroblasts to induced neuronal cells. By deconstructing heterogeneity at each time point and ordering cells by transcriptome similarity, we find that the molecular reprogramming path is remarkably continuous. Overexpression of the proneural pioneer factor Ascl1 results in a well-defined initialization, causing cells to exit the cell cycle and re-focus gene expression through distinct neural transcription factors. The initial transcriptional response is relatively homogeneous among fibroblasts, suggesting that the early steps are not limiting for productive reprogramming. Instead, the later emergence of a competing myogenic program and variable transgene dynamics over time appear to be the major efficiency limits of direct reprogramming. Moreover, a transcriptional state, distinct from donor and target cell programs, is transiently induced in cells undergoing productive reprogramming. Our data provide a high-resolution approach for understanding transcriptome states during lineage differentiation.
Patzke C, Acuna C, Giam LR, Wernig M, Südhof TC
Hundreds of L1CAM gene mutations have been shown to be associated with congenital hydrocephalus, severe intellectual disability, aphasia, and motor symptoms. How such mutations impair neuronal function, however, remains unclear. Here, we generated human embryonic stem (ES) cells carrying a conditional L1CAM loss-of-function mutation and produced precisely matching control and L1CAM-deficient neurons from these ES cells. In analyzing two independent conditionally mutant ES cell clones, we found that deletion of L1CAM dramatically impaired axonal elongation and, to a lesser extent, dendritic arborization. Unexpectedly, we also detected an ∼20-50% and ∼20-30% decrease, respectively, in the levels of ankyrinG and ankyrinB protein, and observed that the size and intensity of ankyrinG staining in the axon initial segment was significantly reduced. Overexpression of wild-type L1CAM, but not of the L1CAM point mutants R1166X and S1224L, rescued the decrease in ankyrin levels. Importantly, we found that the L1CAM mutation selectively decreased activity-dependent Na(+)-currents, altered neuronal excitability, and caused impairments in action potential (AP) generation. Thus, our results suggest that the clinical presentations of L1CAM mutations in human patients could be accounted for, at least in part, by cell-autonomous changes in the functional development of neurons, such that neurons are unable to develop normal axons and dendrites and to generate normal APs.
Hundreds of L1CAM gene mutations have been shown to be associated with congenital hydrocephalus, severe intellectual disability, aphasia, and motor symptoms. How such mutations impair neuronal function, however, remains unclear. Here, we generated human embryonic stem (ES) cells carrying a conditional L1CAM loss-of-function mutation and produced precisely matching control and L1CAM-deficient neurons from these ES cells. In analyzing two independent conditionally mutant ES cell clones, we found that deletion of L1CAM dramatically impaired axonal elongation and, to a lesser extent, dendritic arborization. Unexpectedly, we also detected an ∼20-50% and ∼20-30% decrease, respectively, in the levels of ankyrinG and ankyrinB protein, and observed that the size and intensity of ankyrinG staining in the axon initial segment was significantly reduced. Overexpression of wild-type L1CAM, but not of the L1CAM point mutants R1166X and S1224L, rescued the decrease in ankyrin levels. Importantly, we found that the L1CAM mutation selectively decreased activity-dependent Na(+)-currents, altered neuronal excitability, and caused impairments in action potential (AP) generation. Thus, our results suggest that the clinical presentations of L1CAM mutations in human patients could be accounted for, at least in part, by cell-autonomous changes in the functional development of neurons, such that neurons are unable to develop normal axons and dendrites and to generate normal APs.
De Los Angeles A, Ferrari F, Fujiwara Y, Mathieu R, Lee S, Lee S, Tu HC, Ross S, Chou S, Nguyen M, Wu Z, Theunissen TW, Powell BE, Imsoonthornruksa S, Chen J, Borkent M, Krupalnik V, Lujan E, Wernig M, Hanna JH, Hochedlinger K, Pei D, Jaenisch R, Deng H, Orkin SH, Park PJ, Daley GQ
De Los Angeles A, Ferrari F, Xi R, Fujiwara Y, Benvenisty N, Deng H, Hochedlinger K, Jaenisch R, Lee S, Leitch HG, Lensch MW, Lujan E, Pei D, Rossant J, Wernig M, Park PJ, Daley GQ
Yi F, Danko T, Botelho SC, Patzke C, Pak C, Wernig M, Südhof TC
Heterozygous SHANK3 mutations are associated with idiopathic autism and Phelan-McDermid syndrome. SHANK3 is a ubiquitously expressed scaffolding protein that is enriched in postsynaptic excitatory synapses. Here, we used engineered conditional mutations in human neurons and found that heterozygous and homozygous SHANK3 mutations severely and specifically impaired hyperpolarization-activated cation (Ih) channels. SHANK3 mutations caused alterations in neuronal morphology and synaptic connectivity; chronic pharmacological blockage of Ih channels reproduced these phenotypes, suggesting that they may be secondary to Ih-channel impairment. Moreover, mouse Shank3-deficient neurons also exhibited severe decreases in Ih currents. SHANK3 protein interacted with hyperpolarization-activated cyclic nucleotide-gated channel proteins (HCN proteins) that form Ih channels, indicating that SHANK3 functions to organize HCN channels. Our data suggest that SHANK3 mutations predispose to autism, at least partially, by inducing an Ih channelopathy that may be amenable to pharmacological intervention.
Heterozygous SHANK3 mutations are associated with idiopathic autism and Phelan-McDermid syndrome. SHANK3 is a ubiquitously expressed scaffolding protein that is enriched in postsynaptic excitatory synapses. Here, we used engineered conditional mutations in human neurons and found that heterozygous and homozygous SHANK3 mutations severely and specifically impaired hyperpolarization-activated cation (Ih) channels. SHANK3 mutations caused alterations in neuronal morphology and synaptic connectivity; chronic pharmacological blockage of Ih channels reproduced these phenotypes, suggesting that they may be secondary to Ih-channel impairment. Moreover, mouse Shank3-deficient neurons also exhibited severe decreases in Ih currents. SHANK3 protein interacted with hyperpolarization-activated cyclic nucleotide-gated channel proteins (HCN proteins) that form Ih channels, indicating that SHANK3 functions to organize HCN channels. Our data suggest that SHANK3 mutations predispose to autism, at least partially, by inducing an Ih channelopathy that may be amenable to pharmacological intervention.
Cheloufi S, Elling U, Hopfgartner B, Jung YL, Murn J, Ninova M, Hubmann M, Badeaux AI, Euong Ang C, Tenen D, Wesche DJ, Abazova N, Hogue M, Tasdemir N, Brumbaugh J, Rathert P, Jude J, Ferrari F, Blanco A, Fellner M, Wenzel D, Zinner M, Vidal SE, Bell O, Stadtfeld M, Chang HY, Almouzni G, Lowe SW, Rinn J, Wernig M, Aravin A, Shi Y, Park PJ, Penninger JM, Zuber J, Hochedlinger K
Cellular differentiation involves profound remodelling of chromatic landscapes, yet the mechanisms by which somatic cell identity is subsequently maintained remain incompletely understood. To further elucidate regulatory pathways that safeguard the somatic state, we performed two comprehensive RNA interference (RNAi) screens targeting chromatin factors during transcription-factor-mediated reprogramming of mouse fibroblasts to induced pluripotent stem cells (iPS cells). Subunits of the chromatin assembly factor-1 (CAF-1) complex, including Chaf1a and Chaf1b, emerged as the most prominent hits from both screens, followed by modulators of lysine sumoylation and heterochromatin maintenance. Optimal modulation of both CAF-1 and transcription factor levels increased reprogramming efficiency by several orders of magnitude and facilitated iPS cell formation in as little as 4 days. Mechanistically, CAF-1 suppression led to a more accessible chromatin structure at enhancer elements early during reprogramming. These changes were accompanied by a decrease in somatic heterochromatin domains, increased binding of Sox2 to pluripotency-specific targets and activation of associated genes. Notably, suppression of CAF-1 also enhanced the direct conversion of B cells into macrophages and fibroblasts into neurons. Together, our findings reveal the histone chaperone CAF-1 to be a novel regulator of somatic cell identity during transcription-factor-induced cell-fate transitions and provide a potential strategy to modulate cellular plasticity in a regenerative setting.
Cellular differentiation involves profound remodelling of chromatic landscapes, yet the mechanisms by which somatic cell identity is subsequently maintained remain incompletely understood. To further elucidate regulatory pathways that safeguard the somatic state, we performed two comprehensive RNA interference (RNAi) screens targeting chromatin factors during transcription-factor-mediated reprogramming of mouse fibroblasts to induced pluripotent stem cells (iPS cells). Subunits of the chromatin assembly factor-1 (CAF-1) complex, including Chaf1a and Chaf1b, emerged as the most prominent hits from both screens, followed by modulators of lysine sumoylation and heterochromatin maintenance. Optimal modulation of both CAF-1 and transcription factor levels increased reprogramming efficiency by several orders of magnitude and facilitated iPS cell formation in as little as 4 days. Mechanistically, CAF-1 suppression led to a more accessible chromatin structure at enhancer elements early during reprogramming. These changes were accompanied by a decrease in somatic heterochromatin domains, increased binding of Sox2 to pluripotency-specific targets and activation of associated genes. Notably, suppression of CAF-1 also enhanced the direct conversion of B cells into macrophages and fibroblasts into neurons. Together, our findings reveal the histone chaperone CAF-1 to be a novel regulator of somatic cell identity during transcription-factor-induced cell-fate transitions and provide a potential strategy to modulate cellular plasticity in a regenerative setting.
Kareta MS, Gorges LL, Hafeez S, Benayoun BA, Marro S, Zmoos AF, Cecchini MJ, Spacek D, Batista LF, O'Brien M, Ng YH, Ang CE, Vaka D, Artandi SE, Dick FA, Brunet A, Sage J, Wernig M
Mutations in the retinoblastoma tumor suppressor gene Rb are involved in many forms of human cancer. In this study, we investigated the early consequences of inactivating Rb in the context of cellular reprogramming. We found that Rb inactivation promotes the reprogramming of differentiated cells to a pluripotent state. Unexpectedly, this effect is cell cycle independent, and instead reflects direct binding of Rb to pluripotency genes, including Sox2 and Oct4, which leads to a repressed chromatin state. More broadly, this regulation of pluripotency networks and Sox2 in particular is critical for the initiation of tumors upon loss of Rb in mice. These studies therefore identify Rb as a global transcriptional repressor of pluripotency networks, providing a molecular basis for previous reports about its involvement in cell fate pliability, and implicate misregulation of pluripotency factors such as Sox2 in tumorigenesis related to loss of Rb function.
Mutations in the retinoblastoma tumor suppressor gene Rb are involved in many forms of human cancer. In this study, we investigated the early consequences of inactivating Rb in the context of cellular reprogramming. We found that Rb inactivation promotes the reprogramming of differentiated cells to a pluripotent state. Unexpectedly, this effect is cell cycle independent, and instead reflects direct binding of Rb to pluripotency genes, including Sox2 and Oct4, which leads to a repressed chromatin state. More broadly, this regulation of pluripotency networks and Sox2 in particular is critical for the initiation of tumors upon loss of Rb in mice. These studies therefore identify Rb as a global transcriptional repressor of pluripotency networks, providing a molecular basis for previous reports about its involvement in cell fate pliability, and implicate misregulation of pluripotency factors such as Sox2 in tumorigenesis related to loss of Rb function.
Pak C, Danko T, Zhang Y, Aoto J, Anderson G, Maxeiner S, Yi F, Wernig M, Südhof TC
Heterozygous mutations of the NRXN1 gene, which encodes the presynaptic cell-adhesion molecule neurexin-1, were repeatedly associated with autism and schizophrenia. However, diverse clinical presentations of NRXN1 mutations in patients raise the question of whether heterozygous NRXN1 mutations alone directly impair synaptic function. To address this question under conditions that precisely control for genetic background, we generated human ESCs with different heterozygous conditional NRXN1 mutations and analyzed two different types of isogenic control and NRXN1 mutant neurons derived from these ESCs. Both heterozygous NRXN1 mutations selectively impaired neurotransmitter release in human neurons without changing neuronal differentiation or synapse formation. Moreover, both NRXN1 mutations increased the levels of CASK, a critical synaptic scaffolding protein that binds to neurexin-1. Our results show that, unexpectedly, heterozygous inactivation of NRXN1 directly impairs synaptic function in human neurons, and they illustrate the value of this conditional deletion approach for studying the functional effects of disease-associated mutations.
Heterozygous mutations of the NRXN1 gene, which encodes the presynaptic cell-adhesion molecule neurexin-1, were repeatedly associated with autism and schizophrenia. However, diverse clinical presentations of NRXN1 mutations in patients raise the question of whether heterozygous NRXN1 mutations alone directly impair synaptic function. To address this question under conditions that precisely control for genetic background, we generated human ESCs with different heterozygous conditional NRXN1 mutations and analyzed two different types of isogenic control and NRXN1 mutant neurons derived from these ESCs. Both heterozygous NRXN1 mutations selectively impaired neurotransmitter release in human neurons without changing neuronal differentiation or synapse formation. Moreover, both NRXN1 mutations increased the levels of CASK, a critical synaptic scaffolding protein that binds to neurexin-1. Our results show that, unexpectedly, heterozygous inactivation of NRXN1 directly impairs synaptic function in human neurons, and they illustrate the value of this conditional deletion approach for studying the functional effects of disease-associated mutations.
Chen G, Wernig M, Berninger B, Nakafuku M, Parmar M, Zhang CL
Cell reprogramming technologies have enabled the generation of various specific cell types including neurons from readily accessible patient cells, such as skin fibroblasts, providing an intriguing novel cell source for autologous cell transplantation. However, cell transplantation faces several difficult hurdles such as cell production and purification, long-term survival, and functional integration after transplantation. Recently, in vivo reprogramming, which makes use of endogenous cells for regeneration purpose, emerged as a new approach to circumvent cell transplantation. There has been evidence for in vivo reprogramming in the mouse pancreas, heart, and brain and spinal cord with various degrees of success. This mini review summarizes the latest developments presented in the first symposium on in vivo reprogramming glial cells into functional neurons in the brain and spinal cord, held at the 2014 annual meeting of the Society for Neuroscience in Washington, DC.
Cell reprogramming technologies have enabled the generation of various specific cell types including neurons from readily accessible patient cells, such as skin fibroblasts, providing an intriguing novel cell source for autologous cell transplantation. However, cell transplantation faces several difficult hurdles such as cell production and purification, long-term survival, and functional integration after transplantation. Recently, in vivo reprogramming, which makes use of endogenous cells for regeneration purpose, emerged as a new approach to circumvent cell transplantation. There has been evidence for in vivo reprogramming in the mouse pancreas, heart, and brain and spinal cord with various degrees of success. This mini review summarizes the latest developments presented in the first symposium on in vivo reprogramming glial cells into functional neurons in the brain and spinal cord, held at the 2014 annual meeting of the Society for Neuroscience in Washington, DC.
De Los Angeles A, Ferrari F, Xi R, Fujiwara Y, Benvenisty N, Deng H, Hochedlinger K, Jaenisch R, Lee S, Leitch HG, Lensch MW, Lujan E, Pei D, Rossant J, Wernig M, Park PJ, Daley GQ
Stem cells self-renew and generate specialized progeny through differentiation, but vary in the range of cells and tissues they generate, a property called developmental potency. Pluripotent stem cells produce all cells of an organism, while multipotent or unipotent stem cells regenerate only specific lineages or tissues. Defining stem-cell potency relies upon functional assays and diagnostic transcriptional, epigenetic and metabolic states. Here we describe functional and molecular hallmarks of pluripotent stem cells, propose a checklist for their evaluation, and illustrate how forensic genomics can validate their provenance.
Stem cells self-renew and generate specialized progeny through differentiation, but vary in the range of cells and tissues they generate, a property called developmental potency. Pluripotent stem cells produce all cells of an organism, while multipotent or unipotent stem cells regenerate only specific lineages or tissues. Defining stem-cell potency relies upon functional assays and diagnostic transcriptional, epigenetic and metabolic states. Here we describe functional and molecular hallmarks of pluripotent stem cells, propose a checklist for their evaluation, and illustrate how forensic genomics can validate their provenance.
Lujan E, Zunder ER, Ng YH, Goronzy IN, Nolan GP, Wernig M
In the context of most induced pluripotent stem (iPS) cell reprogramming methods, heterogeneous populations of non-productive and staggered productive intermediates arise at different reprogramming time points. Despite recent reports claiming substantially increased reprogramming efficiencies using genetically modified donor cells, prospectively isolating distinct reprogramming intermediates remains an important goal to decipher reprogramming mechanisms. Previous attempts to identify surface markers of intermediate cell populations were based on the assumption that, during reprogramming, cells progressively lose donor cell identity and gradually acquire iPS cell properties. Here we report that iPS cell and epithelial markers, such as SSEA1 and EpCAM, respectively, are not predictive of reprogramming during early phases. Instead, in a systematic functional surface marker screen, we find that early reprogramming-prone cells express a unique set of surface markers, including CD73, CD49d and CD200, that are absent in both fibroblasts and iPS cells. Single-cell mass cytometry and prospective isolation show that these distinct intermediates are transient and bridge the gap between donor cell silencing and pluripotency marker acquisition during the early, presumably stochastic, reprogramming phase. Expression profiling reveals early upregulation of the transcriptional regulators Nr0b1 and Etv5 in this reprogramming state, preceding activation of key pluripotency regulators such as Rex1 (also known as Zfp42), Dppa2, Nanog and Sox2. Both factors are required for the generation of the early intermediate state and fully reprogrammed iPS cells, and thus represent some of the earliest known regulators of iPS cell induction. Our study deconvolutes the first steps in a hierarchical series of events that lead to pluripotency acquisition.
In the context of most induced pluripotent stem (iPS) cell reprogramming methods, heterogeneous populations of non-productive and staggered productive intermediates arise at different reprogramming time points. Despite recent reports claiming substantially increased reprogramming efficiencies using genetically modified donor cells, prospectively isolating distinct reprogramming intermediates remains an important goal to decipher reprogramming mechanisms. Previous attempts to identify surface markers of intermediate cell populations were based on the assumption that, during reprogramming, cells progressively lose donor cell identity and gradually acquire iPS cell properties. Here we report that iPS cell and epithelial markers, such as SSEA1 and EpCAM, respectively, are not predictive of reprogramming during early phases. Instead, in a systematic functional surface marker screen, we find that early reprogramming-prone cells express a unique set of surface markers, including CD73, CD49d and CD200, that are absent in both fibroblasts and iPS cells. Single-cell mass cytometry and prospective isolation show that these distinct intermediates are transient and bridge the gap between donor cell silencing and pluripotency marker acquisition during the early, presumably stochastic, reprogramming phase. Expression profiling reveals early upregulation of the transcriptional regulators Nr0b1 and Etv5 in this reprogramming state, preceding activation of key pluripotency regulators such as Rex1 (also known as Zfp42), Dppa2, Nanog and Sox2. Both factors are required for the generation of the early intermediate state and fully reprogrammed iPS cells, and thus represent some of the earliest known regulators of iPS cell induction. Our study deconvolutes the first steps in a hierarchical series of events that lead to pluripotency acquisition.
De Los Angeles A, Ferrari F, Fujiwara Y, Mathieu R, Lee S, Lee S, Tu HC, Ross S, Chou S, Nguyen M, Wu Z, Theunissen TW, Powell BE, Imsoonthornruksa S, Chen J, Borkent M, Krupalnik V, Lujan E, Wernig M, Hanna JH, Hochedlinger K, Pei D, Jaenisch R, Deng H, Orkin SH, Park PJ, Daley GQ
Marius Wernig
wernig@stanford.edu
Dr. Marius Wernig is a Professor of Pathology and a Co-Director of the Institute for Stem Cell Biology and Regenerative Medicine at Stanford University. He graduated with an M.D. Ph.D. from the Technical University of Munich where he trained in developmental genetics in the lab of Rudi Balling. After completing his residency in Neuropathology and General Pathology at the University of Bonn, he then became a postdoctoral fellow in the lab of Dr. Rudolf Jaenisch at the Whitehead Institute for Biomedical Research/ MIT in Cambridge, MA. In 2008, Dr. Wernig joined the faculty of the Institute for Stem Cell Biology and Regenerative Medicine at Stanford University where he has been ever since.
He received an NIH Pathway to Independence Award, the Cozzarelli Prize for Outstanding Scientific Excellence from the National Academy of Sciences U.S.A., the Outstanding Investigator Award from the International Society for Stem Cell Research, the New York Stem Cell Foundation Robertson Stem Cell Prize, the Ogawa-Yamanaka Stem Cell Prize delivered by the Gladstone Institute and more recently has been named a Faculty Scholar by the Howard Hughes Medical Institute.
Dr. Wernig’s lab is interested in pluripotent stem cell biology and the molecular determinants of neural cell fate decisions. His laboratory was the first to generate functional neuronal cells reprogrammed directly from skin fibroblasts, which he termed induced neuronal (iN) cells. The lab is now working on identifying the molecular mechanisms underlying induced lineage fate changes, the phenotypic consequences of disease-causing mutations in human neurons and other neural lineages as well as the development of novel therapeutic gene targeting and cell transplantation-based strategies for a variety of monogenetic diseases.
Academic appointments
Associate Professor Institute for Stem Cell Biology and Regenerative Medicine
Member:
Bio-X
Cardiovascular Institute
Child Health Research Institute
Institute for Stem Cell Biology and Regenerative Medicine
Stanford Cancer Institute
Stanford Neurosciences Institute
Administrative appointments
Faculty Senate, Department of Pathology (2017 - Present)
Assistant Professor, Institute for Stem Cell Biology and Regenerative Medicine (2008 - 2014)
Honors & Awards
HHMI Faculty Scholar Award, Howard Hughes Medical Institute (2016)
New York Stem Cell Foundation Robertson Stem Cell Prize, New York Stem Cell Foundation (2014)
The Outstanding Young Investigator Award, International Society for Stem Cell Research (2013)
Ascina Award, Republic of Austria (2010)
Cozzarelli Prize for Outstanding Scientific Excellence, National Academy of Sciences USA (2009)
New Scholar in Aging, Ellison Medical Foundation (2010)
Robertson Investigator Award, New York Stem Cell Foundation (2010)
Donald E. and Delia B. Baxter Faculty Scholarship, Stanford University (2009)
Margaret and Herman Sokol Award, Biomedical Research (2007)
Longterm fellowship Human Frontiers Science Program Organisation, HFSP (2004-2006)
Boards, Advisory Committees
Professional Organizations Member, Society for Neuroscience (2003 - Present)
Member, International Society for Stem Cell Research (2004 - Present)
Editorial Board Member, Cell Stem Cell (2012 - Present)
Editorial Board Member, Stem Cell Reports (2013 - Present)
Member, Program Committee, Society for Neuroscience (2016 - Present)
Chair, Program Committee, International Society for Stem Cell Research (2017 - Present)
Professional Education
M.D., Technical University of Munich, Medicine (2000)
Team

I joined the Wernig lab as an LSRP in the summer of 2022 after graduating from UCLA. I’m interested in the regenerative capabilities of the human body and the molecular mechanisms underlying these regenerative systems, as well as the ways in which we can utilize these mechanisms to treat disease via tools such as cell and gene therapy. My research interests further include immunological topics such as cancer biology and the coevolution of pathogenic species and the immune response. In the Wernig lab, I am investigating methods of replacing dysfunctional microglia in the CNS in the context of neurodegenerative diseases, as well as the translational potential of gene editing and the role that genetically manipulated cells can play in treating such diseases. Outside the lab, I enjoy spending time at the beach, watching sports, and going on road trips with my friends.
Danwei Wu is a Stanford neurology resident in the Neuroscience Scholar Track and aspiring neuroimmunologist. Prior to starting residency, she completed an HHMI Medical Research Fellowship with Dr. Vann Bennett at Duke University studying neuron-specific membrane domains and their interaction with cytoskeletal structures. Her current research interest includes cell-based therapies for multiple sclerosis, molecular pathways of neuro-repair, and pathogenesis of autoimmunity. She is interested in developing new therapies for neurologic diseases. Outside of the lab, she enjoys hiking and reading science fiction.
I am a PhD student in the Neurosciences Interdepartmental Program and joined the lab in summer 2022. I am interested in developing methods to reprogram stem cells directly into oligodendrocytes. I then hope to use these cells to study the role of oligodendrocytes in aging and neurodegeneration. In my free time I like to read, ski, and play tennis.
I am a passionate cellular and molecular biologistwith expertise in research related to cancer, genomic/chromosomal instability, DNA damage response, epigenetics, proteomics and cellular identity. The latter topic attracted me to the Wernig lab where I aim to decipher the mechanisms that allow us to specifically switch the identity of a cell, converting differentiated somatic cells into induced neurons. I also work on a project that aims to integrate CRISPR/CAS9-mediated gene correction with iPS cell generation in order to establish a therapy for the devastating skin disease epidermolysis bullosa. In my free time I play underwater rugby, surf, spearfish and ski!
I am an undergraduate studying neurobiology and computer science. In the Wernig Lab, I am studying how the interactions between reprogramming factors and chromatin modifiers allow for fully developed fibrojacklynl@stanford.edublasts to reprogram into induced neuronal cells (iN).
I studied small GTPase signaling and how its perturbation can contribute to cancer and neurological disorders during my PhD training at Cold Spring Harbor Laboratory. Since then, I have become increasingly fascinated by the epigenetic mechanisms of gene regulation, and how changes in epigenome influence cell function and fate decisions. In the Wernig lab, I am currently investigating the interactions between the reprogramming factors and chromatin modifiers. More specifically, I am interested in finding out how such interactions enable a terminally differentiated cell—for example, a fibroblast—to acquire new transcriptional program that allows its reprogramming into induced neuron (iN).
I am a Bachelor of Science candidate in Bioengineering at Stanford University. My research in the Wernig Lag involves investigating the relationship between microglia and the IKBKAP gene, specifically its role in mechanisms such as microglia regeneration and the transdifferentiation of hematopoietic stem and progenitor cells into microglia-like cells.
Kayla is a PhD student in the Neurosciences Interdepartmental Program and joined the lab in summer 2022. She is interested in leveraging the lab's cell reprogramming techniques to study the roles of individual cell types in proteinopathies. She aims to faithfully recapitulate disease states and uncover the underlying molecular mechanisms that lead to neurodegeneration. In her free time, Kayla can be found birding, hiking, or performing with the Stanford Symphony Orchestra.
I received my BA in molecular and cell biology (Neurobiology focus) and computer science from UC Berkeley. I went on to do my PhD at Duke University, where I worked on engineering electrical synapses for precise neuromodulation in Kafui Dzirasa’s lab. Now, as a postdoc in Marius Wernig lab, I am interested in delving deeper into cellular engineering to better understand neuronal induction, synapse formation, and deliver treatment across the blood brain barrier using engineered microglia. In my free time, I enjoy cooking and coding/electrical engineering projects.
As a neurosurgical resident, my research interests include translational topics such as cell therapy and neuroregenerative mechanisms. In the Wernig lab, I study the cellular reprogramming potential of microglia. Moreover, I’m interested in the functional integration of induced neurons into neural systems.
I am an undergraduate student studying Human Biology. At Wernig Lab, I am helping to research how microglial cells organize and communicate with each other. I am interested in understanding the relationship between changes in the organization of microglia and other neural cells and the progression of neuronal diseases.
I received my Ph.D. in Neuroscience and Brain Technologies in 2021 from the University of Genoa and the Italian Institute of Technology, Italy. I joined the Wernig lab in December 2022. Here, I am interested in understanding how the microglia-derived factors end up in the neuronal lysosomes. Furthermore, I am interested in understanding how the accumulation and breakdown of these factors lead to neurodegenerative disorders using human induced pluripotent stem cell culture. I read non-fiction novels, sketch, and go for hikes in my free time.
Rida Rehman received her doctorate in Natural Sciences (Dr. Rer. Nat.), specializing in brain trauma and rehabilitation at Universtät Ulm, Germany in 2023. She also holds an M.S. in Biomedical Sciences and a B.S. in Applied Biosciences from NUST, Pakistan. Rida’s research has primarily focused on understanding the critical role of microglia in neurotrauma, degeneration, reprogramming and repair. Rida joined Wernig lab in 2023 and is primarily working on microglia to neuron reprogramming.
I worked as a neurologist for 10 years in Japan. During clinical practice, I saw a lot of patients who could not be treated by the current medicine. As a result, I became strongly attracted to basic research of neuroscience. I received my PhD in Dr. Tatsushi Toda’s lab at Kobe University, where I studied disease-modifying drug for Parkinson’s disease. As a post doc fellow in the Wernig lab, I’m interested in investigating the ubiquitylation enzymes that are associated with the pathophysiology of Alzheimer’s disease in order to cure patients with neurodegenerative diseases in the future. In my free time, I play with my children, go cycling, and read comics.
I am a PhD student in the Department of Neurosciences and I joined the Wernig lab in the summer of 2020. I hope to study the fundamental cell biology of microglia giving rise to stable tiling in the brain. Furthermore, I am interested in how these mechanisms contribute to brain homeostasis and change with neuronal disease.
During my PhD in Yongjuan Zhao and Honcheung Lee’s lab, I focused on studying the enzymatic activity and function of ADP-ribosyl cyclase, particularly the activity of SARM1 and its role in axon degeneration. This work sparked my interest in neuroscience and neuropathology. Microglia, the resident immune cells in the brain, play critical roles in neuronal function and can be either beneficial or detrimental in the context of neurodegenerative diseases.In Wernig’s lab, I am interested in investigating the function of microglia in aging and Alzheimer’s disease. My current research focuses on understanding the effects of clonal hematopoietic mutations on microglia and their role in the development of Alzheimer’s disease.
I'm excited about diving into the mysteries of cell fate changes at both the cellular and molecular biology levels, using both experimental and computational tools. In the Wernig lab, I'm on a fascinating journey exploring methods to reprogramm cells into specific neuronal fates. Plus, I'm eager to unravel the basic transcriptional regulation codes in these processes.
Alumni




.gif)

Alan Napole was an LSRP working on elucidating the mechanisms of transgene silencing following iN differentiation from pluripotent stem cells. Concurrently, Alan is also working on understanding the role of microglia in multiple sclerosis via EAE mice models. Previously, he was a CIRM scholar working closely with microglia replacement strategies to develop a human mouse microglia chimera for investigation of neuroimmunological diseases. Alan is currently applying to medical school with interests in neuroscience and surgery. Outside of the lab, he enjoys attending music festivals, playing soccer, and cooking. He moved on to grad school in his home town LA. We wish him all the best for his future endeavors!
Angel earned his B.S. in Biology at California State Polytechnic University, Pomona. As an undergraduate he studied the effects of nicotine on diabetic individuals. As a CIRM fellow at Stanford University, he is interested in using microglia cell replacement and stem cell technology as a potential therapeutic for neurological disorders. Unfortunately, COVID19 cut some of the last of his time he was planning to stay with us. We are proud of Angel that he got into the PhD program at UC Irvine where he moved during these challenging times of natural disasters of the year 2020. Good luck Angel!
Bahareh's research interests were focused on epigenetic regulation of cognition at the level of synapses, using iN system. In my free time she likes to do sports and outdoor activities, cook healthy food, make mixed drinks, play music, and collect vinyl records. After graduating from our Stem Cell and Regenerative Medicine PhD program she moved on as postdoctoral fellow to Boston.
Cheen Euong Ang was a bioengineering PhD student in the Wernig lab. He spent his undergraduate career at McGill University, graduating with a B.Sc. in Chemistry with a focus in biological chemistry. Since coming to Stanford, Cheen Euong has been working on investigating the mechanisms of iN reprogramming and applying the iN platform in disease modeling and aging. Other than doing research in the lab, Cheen Euong has participated several scientific outreach programs such as the Stanford Biomedical Engineering Society undergraduate academic mentoring program and Stanford Institute of Medical Summer High School Student Research Program. Cheen moved on to do his postdoc in Xiaowei Zhuang at Harvard University in Cambridge, MA.
Christian's project focused on the function of synaptic proteins in the context of human neurons. Brain research has made tremendous advances in the last decades using animal models. However, most neuropathological conditions, such as autism or schizophrenia, are unique to human physiology. Thus, I study the effect of genetic alterations of synaptic proteins in induced human neurons using immunohistochemistry, analysis of gene and protein expression, as well as electrophysiology. Christian moved on to a senior lecturer position at the newly formed university of Linz, Austria. Good luck there!
Graduating from UC Berkeley majoring in Biology with an honors in Neuroscience, and having worked as an MD at the Royal Melbourne Hospital, I have developed a particular interest in translational neuroscience. In the lab, I am investigating the efficacy of cell therapies for neurological disorders. I am currently working on microglia based therapies for major neurological diseases, including multiple sclerosis.
I am a molecular biologist with a focus on neuro- and cancer biology. I am interested in using human iPSCs to develop new in vitro disease models, particularly for neuropsychiatric disorders and neurooncology. This led me to the Wernig lab where I started my postdoc to explore the advantages of direct neuronal reprogramming and the intricacies of step-wise differentiation of neural cell types. I am genetically engineering iPSC lines to generate complex genomic alterations and inducible mutations. Following differentiation into the corresponding disease-relevant tissue, I am puzzling together cellular phenotypes, transcriptional regulation, protein interactions, and epigenetic changes for a better understanding of the disease biology. In my spare time, I enjoy a new definition of chaos by my 2-year-old daughter.
Hiroko received Ph.D. from UCLA Neuroscience program in Jim Waschek's lab. She's currently a postdoc studying the disease mechanism of pediatric brain disorder Pelizaeus-Merzbacher Disorder, affecting oligodendrocyte development and myelination. She uses patient-derived iPS cells, gene targeting in iPS cells, and animal models.
I was an administrative associate for the Wernig Lab for a brief period in 2019. I am a native San Franciscan and I love the bay area. I received my undergrad from San Francisco State. I am fluent inSpanish so if you ever need a Spanish lesson come by desk. My husband and I have three beautiful childrenand during my time off I really enjoying spending time with my family.
I grew up in Long Island, NY. I attended college at Cornell University majoring in Biological Sciences with a concentration in Neurobiology and Behavior. After graduation in 2009, I moved to Nashville, TN to join the Medical Scientist Training Program at Vanderbilt University where I earned a combined MD/PhD. In 2016, I started my residency in Neurosurgery at Stanford. In the Wernig lab, I am interested in developing microglia-based regenerative therapies for neurodevelopmental and neurodegenerative disorders.
I received my PhD from National Institute of Biological Sciences (NIBS) at Beijing, China. My PhD mentor is Dr. Xiaodong Wang, who is a chinese-born American biochemist best known for his work with cytochrome C on apoptosis. He is a member of United States National Academy of Sciences and Howard Hughes Medical Institute.
During my PhD stage, my major work is to try and find function of a protein named RIP3 in necrosis (other program cell death) pathway. I use human fetal neural stem cells to study mutation caused epigenetic rigidity in reprogramming process. A lot of patient diseases are caused by gene mutation, but we do not know which kind of cells and which site of mutate will cause disease. We try to work on neural stem cells to induce some point mutation to imitate brain cancer disease from reported mutation site in human patient. Then we will know which mutation site is the key and try to fix it by the biology method.
The immense potential of genetic engineering technology as a tool to understand disease mechanisms and as a therapy motivates me to pursue research. I am studying CRISPR/Cas9 mediated gene correction of mutations in patients suffering from Epidermolysis bullosa. I am also studying iPSC-derived induced neurons to model neurological disorders.
Minjeong was the administrative associate for the Wernig Lab. We all loved her positive spirit that made our lab a happy place. We were fortunate to have her for a full year! During her time off, she loved hanging out with my family and trying out different recipes. She moved on to a full time position in business.
Dr. Moritz Mall is a postdoctoral fellow in the lab. After studying biochemistry and molecular biology at the LMU in Munich and the ETH in Zurich he received his Ph.D. from the EMBL in Heidelberg for his mechanistic studies on mitotic cell division. Besides surfing Moritz’s passion is to understand the molecular mechanisms of cell fate determination during reprogramming, development and disease.
A striking feature of the mammalian nervous system is its enormous cellular diversity. The biological question that drives my research in long-term is to understand how the nervous system develops and achieves its extraordinary complexity. I would also like to leverage my expertise in lineage reprogramming, stem cell biology, and neurobiology to develop reprogramming-based human cell culture models and study the fundamental processes underlying the development and function of human nervous system under normal and pathological conditions. Outside the lab, I like spending my time cycling, rock climbing and hiking.
I grew up in Australia where I completed an undergraduate degree in neuroscience and an MD at the University of Melbourne, Australia. I then completed my intern year at the Royal Melbourne Hospital. I have a keen interest in stem cell therapeutics and their potential application in treating debilitating neurological conditions. My current research focus is on novel microglia based therapies that can potentially ameliorate disease progression in multiple sclerosis.
With billions of neurons interconnected with many billions of synapses, our brain is the most complex object in the known universe. I like to think that I’m doing my part in understanding it. I use human neurons to study a synaptic protein called Neuroligin 4 that is not found in mice, therefore very complicated to study but at the same time extremely fascinating. When mutated Neuroligin 4 causes Autism and impairs the synaptic transmission of neurons. After leaving his prominent imprint on the lab he moved on to join the faculty at Mount Sanai School of Medicine in New York. Good luck Samuele, we will miss you!
My research interest is to investigate how genetic background contributes to the pathomechanism of complex mental disorders such autism or schizophrenia. In order to achieve my goals I am using various experimental techniques including rodent and human neuronal cell culture preparations, immunohistochemistry, gene and protein expression analysis and electrophysiology. As a scientist, my motto is: "We work in the dark to serve the light." Tamas moved back to his home country Hungary.
Virginia is a dentist that worked with underserved communities before taking time off to care for her family. She is happy to be the administrative associate for the Wernig lab. In her free time she enjoys reading, playing tennis, and spending time with her family. Unfortunately, due to COVID19 Virginia needed more time to care for her children and had to leave us. She was a delight to have around and we will dearly miss her!
Wendy received her Ph.D. from Columbia University, where she studied how cholesterol-rich membrane microdomains regulate a distinct function of a transmembrane protein, resulting in specific behavioral outcomes. In the Wernig lab, she aimed to understand the molecular mechanisms by which neuronal identity is established and how its disruption leads to neurological diseases focusing on the gene Myt1l.
Yingfei Liu is a Neurobiology PhD candidate from Xi`an Jiaotong University,China. She is studying here for two years as a Joint-Training Doctoral Program. Her previous research interest was the self-renewal and differentiation of the neural stem cells. Now She is studying the mechanisms of direct lineage reprogramming of fibroblasts into neurons. Yingfei was great to have in the lab. COVID19 also affected Yingfei's carreer. In the midst of great progress COVID19 precluded much of her continuing to work. She went back to China to arrange for her PhD defense and we are hoping to be able to continue to work with her in the future. Good luck Yingfei!
I completed my PhD in Dr. TY Chang’s lab at Dartmouth College, where I studied cholesterol metabolism in health and disease. In the Wernig lab, my research focus is on studying neurological diseases in human neurons and other neural lineages. I am also interested in developing novel therapeutic approaches for treating incurable neurological disorders using reprogramming technology.
Yongjin received his Ph.D. in functional genomics in 2018 from the Seoul National University, South Korea. For his Ph.D., he focused on genetic mutations of human neurological patients and its functional impacts. Yongjin joined the Wernig lab in October 2018. In the Wernig lab, he is interested in developing therapeutic methods for neurological patients and understanding disease mechanisms using human stem cells and neurons. We are proud that Yongjin accepted an offer to join the faculty at the prestigious Seoul University.
Press
Wernig Lab Protocols & Recipes
Contact
We are always interested to hear from ambitious scientists and potential collaborators.
Marius Wernig
wernig@stanford.edu
Amy Lang, Lab Admin
alang2@stanford.edu
Institute for Stem Cell Biology and Regenerative Medicine
Wernig Laboratory
265 Campus Drive G3141
Stanford, CA 94305
U.S.A.

